Many people turn to bariatric surgery as a last resort of weight loss to improve health and quality of life. Since, past attempts at losing weight have been unsuccessful or not successful long term, bariatric surgery has become more of an accepted form of weight loss.
Bariatric surgery is performed in overweight and obese adults to promote rapid weight loss. It is a tool that, combined with a healthy diet, exercise, and lifestyle choices, allows people to achieve long-term weight loss success. There are several positive outcomes of weight loss surgery, including an improvement in many overweight and obesity-related conditions. Renew Bariatrics’ bariatric surgeons located in Mexico will uncover if bariatric surgery procedures, such as gastric bypass and gastric sleeve, can improve your heart health?
First, let’s see how obesity affects overall health and the heart in particular.
What’s the Connection Between Weight and Health?
To state that there is a strong connection between one’s weight and their overall health is an understatement; in many instances, it represents a direct link, a fundamental relationship that underscores the profound impact of body weight on a myriad of health outcomes. This connection is especially evident in the context of chronic diseases such as Type 2 diabetes, hypertension, cardiovascular diseases, and certain forms of cancer, where excess body weight often plays a pivotal role in the onset, progression, and management of these conditions.
Excess body weight, particularly in the form of obesity, is not merely a matter of aesthetic concern but a significant risk factor that can exacerbate the severity of existing health issues and precipitate the development of new ones. The mechanisms through which excess weight influences health are complex and multifaceted, involving metabolic, hormonal, and inflammatory pathways.
Obesity is a medical condition characterized by an excessive accumulation of body fat, to the extent that it may have a negative impact on health, leading to reduced life expectancy and/or increased health problems. In the United States alone, it is estimated that approximately 97 million adults are classified as either overweight, with a Body Mass Index (BMI) ranging from 25 to 29.9, or obese, with a BMI of 30 or above. This staggering statistic underscores a growing public health crisis that extends beyond national borders, affecting populations worldwide and contributing to a myriad of health complications and chronic diseases.
BMI to Test Weight Status
The BMI is a widely used tool to categorize weight status. It is calculated by dividing a person’s weight in kilograms by the square of their height in meters. While it provides a useful general indication of healthy and unhealthy weight ranges, it does not directly measure body fat percentage or distribution, which can vary significantly among individuals with the same BMI. Despite its limitations, BMI remains a key metric for identifying individuals at risk due to excess body weight.
Health diagnosis
Obesity can be associated with several medical diagnosis, including diabetes, hypertension, respiratory disorders, heart disease, gallbladder disease, kidney disease, liver disease, sleep apnea, cancer, and bone and joint complications.
Facing these prognosis can be alarming, and one significant reason why people turn to major surgery to help find a solution for health and weight concerns.
The good news is that no matter what you weigh, even a modest weight loss of 5-10 percent of your body weight can result in health benefits and decrease the risk of chronic diseases related to obesity.
How Does Obesity Affect the Heart?
What does it actually mean to have heart disease or a heart condition?
Heart disease encompasses a broad term that is utilized to categorize a diverse array of medical conditions that impact the functionality and overall health of the heart muscle. This term includes several complications such as coronary artery disease, which involves the narrowing or blockage of the coronary arteries, heart attacks, arrhythmias (irregular heartbeats), heart failure, and other heart-related irregularities and dysfunctions. The heart, being central to the body’s circulatory system, plays a critical role in sustaining life by pumping blood throughout the body, supplying oxygen and nutrients to tissues, and removing carbon dioxide and other wastes.
Relationship Between Excess Weight & Heart Disease
The relationship between retaining excess weight and the development of heart disease is both direct and multifaceted. Excess body weight, particularly obesity, poses significant challenges to the heart’s ability to perform its essential biological functions. One of the primary concerns is the negative impact on the heart’s efficiency in pumping blood to various parts of the body. The heart of an individual carrying excess weight must work harder to circulate blood, which can lead to an increase in heart rate and blood pressure. Over time, this increased workload can weaken the heart muscle, potentially leading to heart failure, a condition where the heart is unable to pump blood effectively.
Moreover, excess weight can hinder the heart’s ability to receive blood. The increased demand for nutrients and oxygen by the larger body mass, coupled with potential obstructions or narrowing in the coronary arteries due to atherosclerosis (a condition characterized by the buildup of fats, cholesterol, and other substances in and on the artery walls), can strain the heart’s capacity to receive the blood it requires for proper functioning.
Furthermore, and distressing heart disease is the leading cause of death in the United States.
Cardiovascular Diagnosis
Being overweight or obese is a risk factor for many heart conditions such as high blood pressure, heart attack, abnormal heart rhythm, angina and heart failure. Increased body fat directly contributes to heart disease by causing atherosclerosis (plaque build-up in the arteries) and enlargement of the heart chambers.
Obesity indirectly contributes to heart disease by causing sleep apnea (starting and stopping of breathing during sleep) and thromboembolic disease (clot formation in the bloodstream). Additionally, obesity can worsen or cause many conditions that are risk factors for heart disease, such as high cholesterol and diabetes.
With these threatening symptoms looming, it is important that patients take the proper steps to reduce weight and improve health conditions.
What Does Bariatric Surgery Achieve?
Bariatrics Surgery Explained
Bariatric surgery such as; Gastric Bypass or Gastric Sleeve, works by changing the anatomy of the stomach and digestive system. The surgeries help to reduce the amount of food and liquids that the stomach can hold, by removing a portion of the stomach or bypassing a large portion of the stomach. Bariatric surgery is the strongest “tool” for weight loss. It is designed as a drastic change in one’s ability to eat large portions of food and fall victim to further weight gain.
The profound impact of bariatric surgery extends well beyond the immediate physical alterations to the digestive system. One of the most significant effects of this surgical intervention is its ability to modulate various hormonal levels within the body, which plays a crucial role in regulating hunger, appetite, and the sensation of fullness or satiety. By influencing these hormonal pathways, bariatric surgery can lead to a substantial reduction in hunger and appetite, while simultaneously enhancing the feelings of satiety after smaller meal portions. This dual action effectively addresses one of the primary challenges faced by individuals struggling with obesity: the constant battle against hunger and the tendency to consume large portions of food.
The surgery’s ability to alter the body’s hormonal environment includes changes in key hormones such as ghrelin, often referred to as the “hunger hormone,” which is known to stimulate appetite. Post-surgery, patients typically experience a significant decrease in ghrelin levels, leading to a reduced desire to eat. Additionally, increases in other hormones that promote feelings of fullness and satisfaction after eating, such as peptide YY (PYY) and glucagon-like peptide-1 (GLP-1), contribute to the patient’s ability to feel satisfied with much smaller quantities of food than they would have previously consumed.
To aim for long term weight loss success, it is important to combine with favorable nutrition, regular exercise and reshaping behaviors.
Bariatric Surgery Benefits
Undergoing successful weight loss surgery can markedly enhance an individual’s health status and elevate their overall quality of life. This improvement is not merely limited to the visible aspects of weight reduction but extends deeply into the regulation and control of critical health markers such as blood pressure, blood sugar, and cholesterol levels. The positive changes brought about by significant weight loss can lead to a substantially reduced dependency on medications previously required to manage these conditions, offering a more natural and holistic approach to health maintenance.
The impact of weight loss surgery on blood pressure is profound. Hypertension, or high blood pressure, is a common ailment among individuals struggling with obesity. It places an undue strain on the cardiovascular system, increasing the risk of heart disease, stroke, and kidney damage. Weight loss surgery can lead to a significant reduction in body weight, which in turn can decrease the volume of blood the heart needs to pump, effectively lowering blood pressure. Many patients find that their hypertension becomes much easier to manage after surgery, with some even experiencing normal blood pressure levels without the need for medication.
Does Weight Loss Surgery Lower the Risk of Heart Disease?
Researchers have compared patients who have had weight loss surgery to patients with similar medical status who did not undergo bariatric procedures. The results indicate that procedures such as gastric bypass and gastric sleeve can reduce the risk of obesity-related complications such as coronary artery events (heart attack), heart failure, and atrial fibrillation (heart rhythm abnormalities).
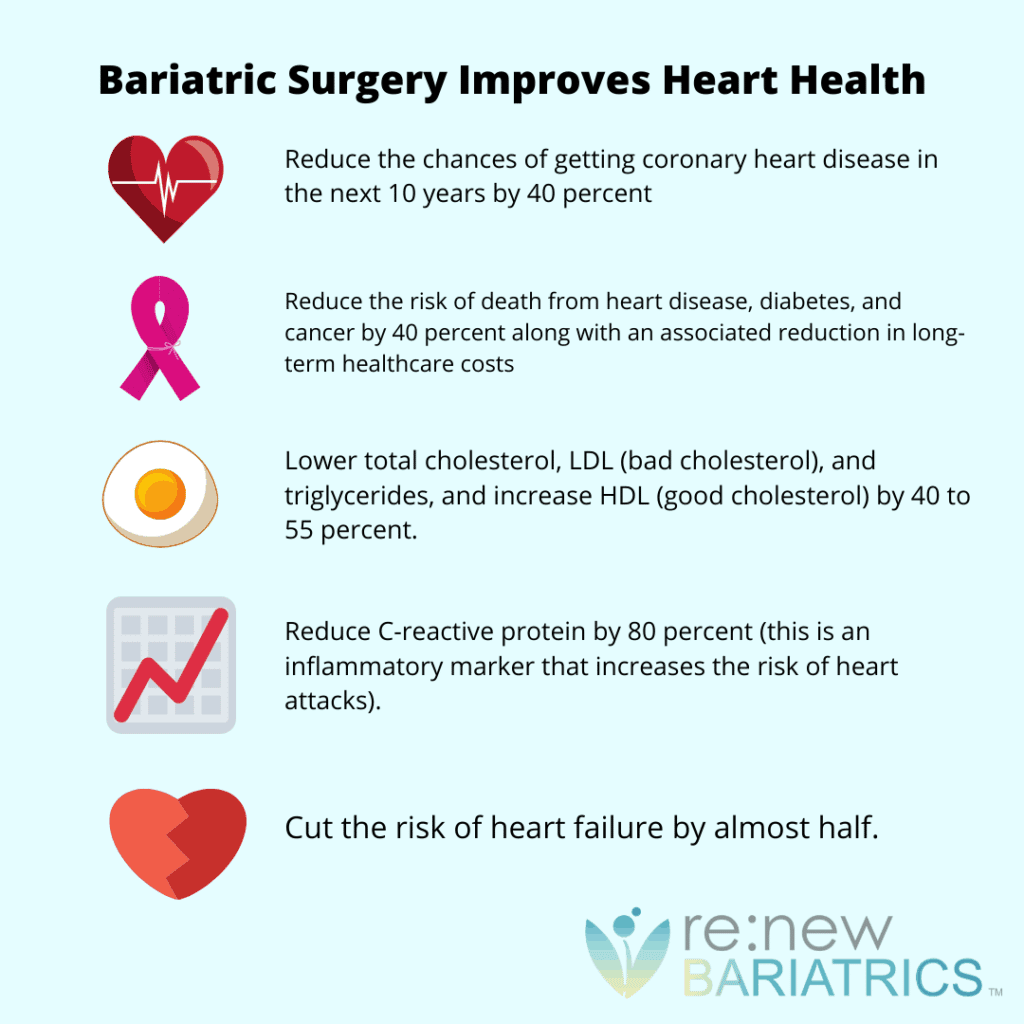
Studies show that weight loss surgery can:
- Reduce the chances of getting coronary heart disease in the next 10 years by 40 percent.
- Lower total cholesterol, LDL (bad cholesterol), and triglycerides, and increase HDL (good cholesterol) by 40 to 55 percent.
- Reduce C-reactive protein by 80 percent (this is an inflammatory marker that increases the risk of heart attacks).
- Cut the risk of heart failure by almost half.
- Reduce the risk of death from heart disease, diabetes, and cancer by 40 percent along with an associated reduction in long-term healthcare costs.
How Heart Health is Impacted By Weight
The connection between carrying excess weight and the state of one’s heart health, along with a multitude of other serious health conditions, is not merely coincidental but profoundly direct and consequential. This relationship underscores a critical health dynamic, where the accumulation of excess body fat significantly elevates the risk of developing cardiovascular diseases, including hypertension, coronary artery disease, heart failure, and stroke, among others. Moreover, the implications of obesity extend beyond the cardiovascular system, implicating a host of other serious health conditions such as Type 2 diabetes, certain forms of cancer, osteoarthritis, and sleep apnea, to name a few.
Excess body weight, particularly in the form of visceral fat that accumulates around the midsection, poses a multifaceted threat to heart health. This type of fat is metabolically active, secreting inflammatory substances and hormones that can lead to atherosclerosis—a condition characterized by the hardening and narrowing of the arteries due to plaque buildup. This process not only impedes blood flow but also strains the heart, compelling it to work harder to pump blood through constricted vessels, thereby increasing the risk of heart attack and stroke.
Disconcerting statistics
Heart disease is responsible for 1 in every 4 deaths and takes the lives of 630,000 Americans every year.
“Heart failure is on the rise, affecting more than 6 million U.S. adults as of 2014. By 2030, that number is expected to surpass 8 million. It’s also a drain on quality of life, causing symptoms such as shortness of breath and fatigue.”
By taking definitive actions to control obesity through weight loss surgery, patients can lower their risk of heart disease and take control of their overall health.
Curious About How Bariatric Surgery Can Improve Your Health?
Contact Renew Bariatrics in Mexico, with bariatric clinics in Tijuana, Mexico and Cancun, Mexico, to find out if you’re a candidate.


