Diabetes and Weight Loss Surgery Statistics
Let’s explore Type 2 Diabetes weight loss statistics, with a focus on bariatric surgery. This surgical intervention, renowned for its efficacy in weight management, reveals additional dimensions when addressing individuals grappling with type 2 diabetes or those struggling on the brink of pre-diabetes.
Type 2 Diabetes affects over three million Americans each year. As obesity rates have rises, so has the paralleling prevalence of Type 2 Diabetes. Bariatric surgery has become a pivot role in helping with weight reduction and contribution to the control of Type 2 Diabetes.
Type 2 Diabetes
“Although small trials have shown benefits to blood glucose control in patients with type 2 diabetes and high BMI, there isn’t enough evidence for people with BMIs lower than 35,” from the American Diabetes Association. This suggests the impacts of bariatric surgery might have more impacts with those with at least a 35 body mass index.
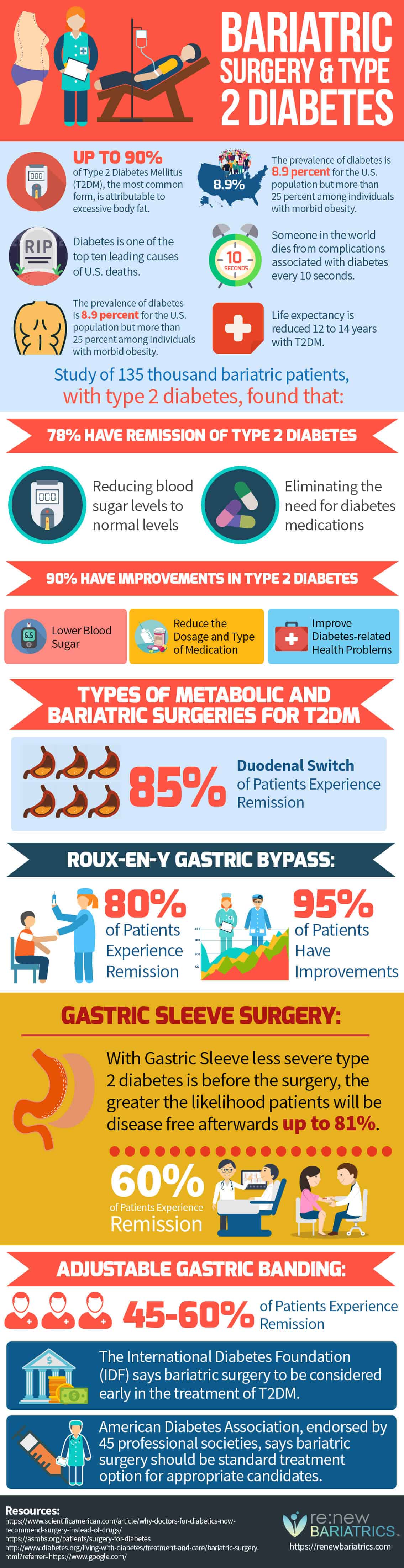
- Up to 90% of Type 2 Diabetes Mellitus (T2DM), the most common form, is attributable to excess body fat.
- The prevalence of diabetes is 8.9 percent for the U.S. population but more than 25 percent among individuals with morbid obesity.
- Diabetes is one of the top ten leading causes of U.S. deaths.
- Someone in the world dies from complications associated with diabetes every 10 seconds.
- The prevalence of diabetes is 8.9 percent for the U.S. population but more than 25 percent among individuals with morbid obesity.
- Life expectancy is reduced 12 to 14 years with T2DM.
Bariatric Patient Study of 135,000 Patients
In a comprehensive study encompassing 135,000 bariatric patients grappling with type 2 diabetes, compelling findings have emerged, shedding light on the significant impact of bariatric surgery on diabetes management. The study reveals that an impressive 78% of these patients experienced remission of type 2 diabetes post-surgery.
This remission translates to a normalization of blood sugar levels, reaching a state where the need for diabetes medications becomes obsolete. It underscores the transformative potential of bariatric surgery in not only addressing weight concerns but also in effectively mitigating the core metabolic issues associated with type 2 diabetes.
The study highlights that a staggering 90% of the bariatric patients observed improvements in their type 2 diabetes condition. These enhancements encompassed lower blood sugar levels, allowing for a reduction in the dosage and even a change in the type of diabetes medication required.
These positive outcomes extended to improve various health problems linked to diabetes, further emphasizing the multiple benefits of bariatric surgery in enhancing the overall health of individuals who struggle with with type 2 diabetes. The findings from this extensive patient study focusing on the potential of bariatric surgery aiding in the management of type 2 diabetes.
How Does Bariatric Surgery Help With Type 2 Diabetes?
Bariatric surgery, also known as weight loss surgery, can significantly help individuals with Type 2 diabetes, often leading to improvement or remission of the disease. The mechanisms through which bariatric surgery aids in the management of Type 2 diabetes are multifaceted and include both immediate and long-term effects. Here’s how bariatric surgery helps with Type 2 diabetes:
- Weight Loss: The most direct impact of bariatric surgery is significant weight loss. Losing a substantial amount of weight improves insulin sensitivity, meaning the body can use insulin more effectively to lower blood sugar levels. This reduction in body weight also decreases the fat deposits in the liver and pancreas, which can help these organs function better in managing blood glucose levels.
- Hormonal Changes: Bariatric surgery induces changes in various gut hormones that are involved in hunger and satiety, insulin production, and glucose metabolism. For example, after surgery, levels of the hormone glucagon-like peptide-1 (GLP-1) increase. GLP-1 improves insulin secretion and lowers blood sugar levels. Additionally, reductions in ghrelin, the “hunger hormone,” can decrease appetite and food intake, supporting weight loss and improved blood glucose control.
- Alterations in Gut Microbiota: The surgery can lead to changes in the composition of the gut microbiota, which may have beneficial effects on metabolic regulation, including improved glucose homeostasis and insulin sensitivity.
- Improvements in Insulin Sensitivity and Beta-Cell Function: Bariatric surgery can lead to early improvements in insulin sensitivity, even before significant weight loss occurs. This suggests that mechanisms beyond weight loss contribute to the beneficial effects on diabetes. There’s also evidence that the surgery can help preserve or improve the function of beta cells in the pancreas, which are responsible for insulin production.
- Caloric Restriction and Nutrient Malabsorption: Certain types of bariatric surgery, such as Roux-en-Y gastric bypass and biliopancreatic diversion, not only reduce the stomach size but also alter the digestive system. This can lead to reduced nutrient absorption and caloric intake, which further supports weight loss and improves blood sugar levels.
- Lifestyle Changes: Although not a direct effect of the surgery itself, the significant weight loss and dietary restrictions following bariatric surgery often lead to healthier lifestyle choices, including improved diet and increased physical activity. These changes can further enhance blood glucose control and overall health.
Which Bariatric Procedures Provide the Best Remission Chances for T2DM?
Gastric bypass (RYGB) and sleeve gastrectomy are bariatric procedures that show significant potential for remission of Type 2 diabetes (T2DM). These surgeries induce weight loss and beneficial changes in gut hormones, leading to improved insulin sensitivity.
Gastric bypass surgery stands out as a noteworthy intervention, showcasing high rates of diabetes remission among individuals who undergo the procedure. This surgical approach not only yields significant weight loss but also demonstrates a remarkable impact on diabetes management, with improvements often observed shortly after the surgery. The transformative effects of gastric bypass on diabetes remission underscore its efficacy in addressing the metabolic complexities associated with type 2 diabetes.
Gastric Sleeve surgery, another bariatric surgical procedure, also shows positive outcomes in managing diabetes. While the rates of remission may be slightly lower compared to gastric bypass, this surgical option proves to be a viable and effective means of addressing both weight concerns and diabetes-related issues. The positive effects of sleeve gastrectomy on diabetes further highlight the versatility of bariatric surgery in promoting holistic health improvements.
Duodenal Switch
85% of Patients Experience Remission With Duodenal Switch
The Duodenal Switch (DS) is a type of weight loss surgery designed to address severe obesity by combining restrictive and malabsorptive elements. During the procedure, a significant portion of the stomach is removed to restrict food intake, and the small intestine is rearranged to reduce the absorption of calories and nutrients.
This dual mechanism aims to induce weight loss by both limiting the amount of food the patient can consume and minimizing the absorption of nutrients from that food. The DS is often considered for individuals with a high body mass index (BMI) and obesity-related health issues, offering a more comprehensive and sustainable approach to weight loss compared to other bariatric surgeries.
Roux-en-y Gastric Bypass
80% of Patients Experience Remission With Gastric Bypass
95% of Patients Have Improvements With Gastric Bypass
Gastric bypass surgery, also known as Roux-en-Y gastric bypass (RYGB), is a common and effective weight loss procedure designed to help individuals with obesity achieve significant and sustainable weight reduction. During the surgery, a small pouch is created by dividing the stomach, restricting its capacity and thereby limiting the amount of food a person can eat. Additionally, a section of the small intestine is rerouted and attached to the newly formed stomach pouch, diverting food away from the upper part of the small intestine.
This rearrangement not only reduces calorie absorption but also alters the hormonal signals related to hunger and satiety. Gastric bypass not only facilitates weight loss but often leads to improvements in obesity-related health conditions such as type 2 diabetes and hypertension. While it is a highly effective and well-established procedure, it requires a commitment to lifestyle changes and ongoing medical monitoring for optimal results.
Gastric Sleeve Surgery
60% of Patients Experience Remission With Gastric Sleeve
Gastric sleeve surgery, or sleeve gastrectomy, is a weight loss procedure that involves the removal of a large portion of the stomach, creating a banana-shaped or sleeve-like structure. This reduction in stomach size restricts the amount of food a person can eat, leading to decreased calorie intake and subsequent weight loss. Unlike gastric bypass, the gastric sleeve procedure does not involve rerouting the intestines.
By removing a significant part of the stomach, the surgery not only limits the quantity of food intake but also reduces the production of ghrelin, a hormone associated with hunger. This hormonal and anatomical change contributes to the effectiveness of gastric sleeve surgery in promoting weight loss.
With Gastric Sleeve, less severe type 2 diabetes is before the surgery, the higher the likelihood patients will be disease free afterward up to 81%. Learn more about the benefits of gastric sleeve procedure here.
Adjustable Gastric Banding
45-60% of Patients Experience Remission With Gastric Banding
Adjustable gastric band surgery is a weight loss procedure that involves placing an inflatable silicone band around the upper part of the stomach, creating a small pouch. The band is connected to a port that allows for adjustments to control the size of the opening between the pouch and the rest of the stomach. By restricting the passage of food, the adjustable gastric band induces a feeling of fullness with smaller meals, promoting reduced calorie intake and subsequent weight loss.
One advantage of this procedure is its reversibility, as the band can be adjusted or removed if necessary. However, it requires regular follow-up visits for adjustments and may not be as effective as other bariatric surgeries in achieving significant and sustained weight loss.

The Role of Bariatric Procedures in Type 2 Diabetes Remission
Gastric bypass (RYGB) and sleeve gastrectomy represent two prominent bariatric procedures that hold considerable promise in fostering the remission of Type 2 diabetes (T2DM). These surgical interventions extend beyond their primary goal of inducing weight loss, as they elicit favorable alterations in gut hormones and metabolic pathways, subsequently enhancing insulin sensitivity.
The intricate interplay between these procedures and metabolic regulation underscores their potential as comprehensive solutions for individuals grappling with T2DM. Gastric bypass, renowned for its effectiveness in achieving weight loss, emerges as a frontrunner in the realm of diabetes remission.
This procedure demonstrates high rates of success in alleviating T2DM, often yielding positive outcomes shortly after surgery. The mechanisms underlying the success of gastric bypass involve not only the physical restriction of food intake but also intricate hormonal changes that contribute to improved glucose metabolism and insulin sensitivity.
The resulting impact on insulin sensitivity and glucose regulation makes sleeve gastrectomy an effective option for individuals seeking comprehensive improvements in both weight management and diabetes control. In essence, the nuanced effects of these bariatric procedures extend beyond mere weight reduction, delving into the intricacies of metabolic modulation and hormonal changes. The choice between gastric bypass and sleeve gastrectomy depends on various factors, including individual health profiles, preferences, and specific risk considerations.